This is latest information from PCUK about potential screening service. Source: https://prostatecanceruk.org/about-us/news-and-views/2022/04/why-don-t-we-invite-all-men-for-a-prostate-cancer-test
Many prostate cancers are life-threatening. We know it kills close to 12,000 men in the UK every year. But there are some prostate cancers which have a very small chance of ever impacting your life. For those prostate cancers, you’d probably rather not know about them at all.
This becomes even more important when you consider that treatments for prostate cancer can leave many men experiencing life-long side effects like incontinence or erectile dysfunction. Not to mention the anxiety that having a cancer diagnosis can cause. So for cancers that are unlikely to cause harm, it might be better not to know and to avoid unnecessary treatment and the associated side effects.
The PSA test: saving lives but not good enough for screening
The PSA test is the first test men have for prostate cancer. It’s a blood test that measures the amount of a protein, called Prostate Specific Antigen, released by prostate cells into the blood. PSA is released by healthy cells and it’s normal for PSA levels to gradually increase as the prostate enlarges with age. But if the prostate has cancer, it’s likely there will be a faster increase in the number of cells in the prostate, causing PSA levels to rise more dramatically.
Clinical trials have shown us that using the PSA test to identify prostate cancer can save lives. It’s why we provide so much information to help men understand their risk, understand the PSA test and support them to get the test if they make an informed decision that it’s right for them. This is especially important for men at high risk. That’s why we joined forces with the NHS to find the 14,000 men who have undiagnosed prostate cancer due to the pandemic.
But the PSA test has its flaws. Not all prostates release the same amount of PSA, so a normal score for one man could prevent us finding cancer in another. We know from other research that as many as 1 in 7 men with prostate cancer may have a PSA that is deemed ‘normal’, so a PSA test would miss their cancers entirely. PSA also can’t differentiate between low-risk cancer that may never cause any harm, and aggressive disease that requires treatment.
Thanks to previous research breakthroughs, the diagnostic pathway for prostate cancer is very accurate at knowing which prostate cancers need treating – but right now to get to that accurate diagnosis requires an initial triage with the PSA test, followed by an mpMRI, then a biopsy.
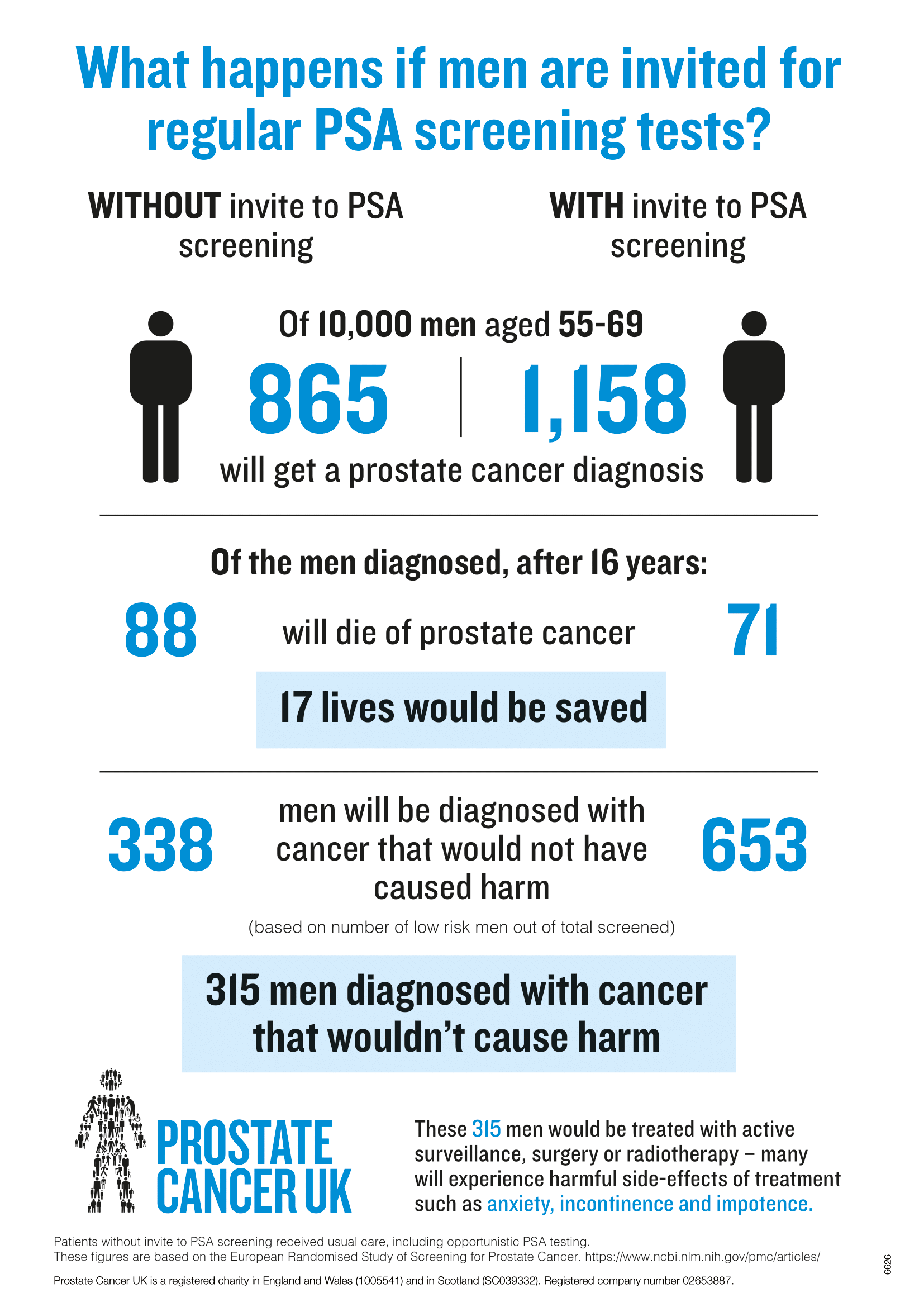
If we were to use the PSA tests in a national screening programme, lots of cancer would be caught earlier, and some lives would be saved, but far more men will have multiple tests, and potential side effects from a biopsy, only to be told they don’t have cancer or that the cancer they have will never cause them harm. Some of these men may also go through unnecessary treatments for a cancer that would never have impacted their life. This is why, even though PSA-based screening has been tested and shown to save lives, it hasn’t been approved by the UK’s National Screening Committee.
We’ve analysed the latest results from a massive European screening trial and summarised them in the infographic shown below.
The PSA test saves lives, but it’s not good enough for screening. To deliver a UK wide screening programme for prostate cancer, we need a simple, quick test that can better identify the men most likely to have harmful cancer that needs further investigation.
The next step: find a better test
We desperately want to bring men a screening programme for prostate cancer and save more lives while doing less harm. To do that, we need new tests. New tests need solid evidence, and that means research. That’s why we’ve committed to making our biggest ever research investment to fund the research that will develop and provide the evidence for new and better tests.
We’re asking researchers to apply for funding to transform prostate cancer diagnosis. They’ll have to answer three crucial questions as part of their application:
- How should we test men?
There are lots of different types of tests, or combinations of tests, that could be used to screen men for prostate cancer. These range from scanning men’s prostates in an MRI scanner, to blood tests or even urine samples. We want researchers to test the best of these methods in the same clinical trial. This approach of testing multiple options at once will help maximise our chance of success in the shortest possible time.
- Which men should we screen?
A screening programme must balance the benefit of catching cancer early with the potential harm of diagnosing cancer that doesn’t require treatment. The best way to do this is to only screen a selection of the population that is at highest risk of the disease – again, just like how women at high risk are invited for breast cancer screening below the age of 50.
We want our researchers to find a way to select the men who are most likely to benefit. For example, we already know black men have an increased risk of prostate cancer, so the trial will need to include enough black men to make sure any new diagnosis pathway is effective for this group of men.
- How can we use the data to keep answering important questions for men?
We need radical change to transform the way prostate cancer is diagnosed. This research will need to involve more men and collect more data than any of our other projects to date.
We want to make the most of this unique opportunity by asking our researchers to take samples like blood, saliva and urine from the men in the trial. These samples should be made available to other researchers around the world so they can answer new questions about prostate cancer, or help improve diagnosis beyond this initial study.

When can we expect a screening programme?
It’s difficult to say how long research like this will take. These proposals will go through a rigorous selection process by independent experts – including other researchers, clinicians and men with prostate cancer – to make sure we fund only the most promising research with the biggest potential to improve diagnosis.
The experts that approve changes to clinical practice need to be absolutely sure that any new test or method for diagnosing men can save lives without causing too much harm. To do this, we need to monitor the men in the trial for several years. That would prove that our new test (or set of tests) really does diagnose more men’s aggressive, harmful cancers early and accurately. And we’ll need to wait for this to happen in big enough numbers so we know it hasn’t happened by chance.
If our research provides a new way of diagnosing prostate cancer that can do all of that, we’ll ask the UK National Screening Committee to analyse the results. They’ll be looking to see if the evidence is enough to change the way we diagnose prostate cancer, and to introduce a screening programme. We’ll continue to fund research until we find a way to diagnose men earlier and more accurately. Once we find it we’ll work with the NHS and other decision makers to make sure that a screening programme can be rolled out across the UK.
Diagnosis for prostate cancer needs radical change. And radical change needs radical investment. We are the only organisation with the focus and expertise to push this research programme into existence. And this research is only possible thanks to the people like you who donate to support our work. Thank you.
Thank you for your ongoing support in our mission towards a screening programme for prostate cancer. Every donation gets us one step closer.


